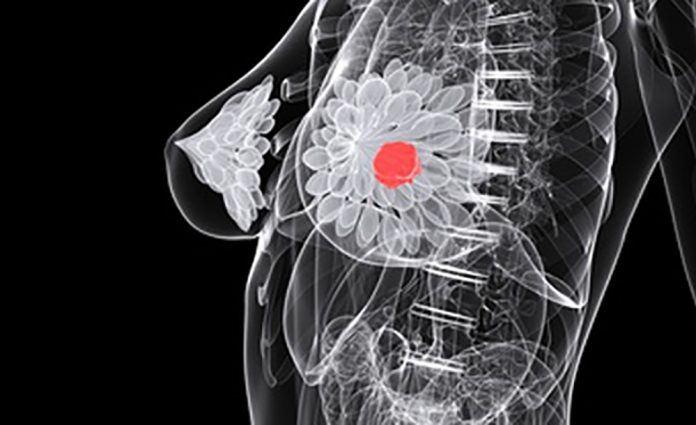
Fat cells, or adipocytes, that grow in close proximity to breast cancers can turn into other cell types that promote tumor growth, a new study by University of Texas (UT) Southwestern researchers suggests.
The findings, published in Cell Reports, could lead to new ways to fight breast cancer, a disease that is diagnosed in more than 300,000 women each year and kills nearly 45,000 annually in the US alone.
“We identified novel adipocyte-derived cell types in the mammary gland that offer a fertile soil for breast cancer tumor invasion and growth,” said study leader Philipp Scherer, professor of Internal Medicine and Cell Biology and a member of the Harold C. Simmons Comprehensive Cancer Center at UTSW.
Obesity has long been considered a risk factor for breast cancer occurrence and worse prognosis. But the relationship between obesity and breast cancer is poorly understood.
Studies have shown that fat cells in close contact with breast tumor cells have an enhanced ability to break down their lipids to provide fuel for invading tumor cells. However, Scherer explained, it has been unclear what other roles these adipocytes play in breast cancer progression.
To answer this question, Qingzhang Zhu, PhD, an instructor of Internal Medicine and member of the Scherer laboratory, and his colleagues tagged adipocytes in lab mice with a fluorescent color, making it possible to follow these cells long term.
Tumor stroma comprise an extensive heterogeneous tissue containing many cell types beyond tumor stem cells, including fibroblasts, epithelial, and immune cells. The cellular responses and metabolic reprograming in the stroma form a unique microenvironment favoring tumor growth.
When the researchers implanted breast tumors in the mice or genetically manipulated the rodents’ own breast cells to turn them into tumor cells, they saw that nearby fat cells shrank and took on forms different from native adipocytes. Genetic testing to identify which genes were active in these fat cells showed they first regressed to an earlier stage in development, then gradually developed genetic markers of other cell types, including connective tissue cells, muscle cells, and immune cells.
“These chemical signals are most likely either growth factors or cytokines, and the identification and characterization of these factors are the next steps that we are embarking on,” Scherer told Inside Precision Medicine.
He adds that, “We infer the existence of these factors at the local interface between infiltrating tumor cells and adjacent fat cells that shrink their lipid content and morph into fibroblast-like cells. The trans-differentiation into other cell types must be tumor-induced by locally acting factors, as you cannot observe these changes in the absence of a tumor.”
Further investigation by this team showed these changed fat cells encouraged breast cancer tumors to grow. However, this property also depended critically on their ability to supply energy to neighboring tumor cells. In addition, the properties of the cell types that fat cells morph into after they lose their lipids and their fat cell identity play a role, since they add significantly to the local fibrosis, which contributes to the stiffness of breast tissue.
When the researchers enhanced the lipid-storing capacity of mature fat cells, they ceased to morph into other cell types and no longer promoted tumor growth.
Scherer said the mechanism for how adipocytes change into other cell types is not yet clear. However, a chemical signal from tumor cells is probably responsible. He and his colleagues plan to search for this signal and look for other ways to manipulate this system to discourage breast cancer growth.













